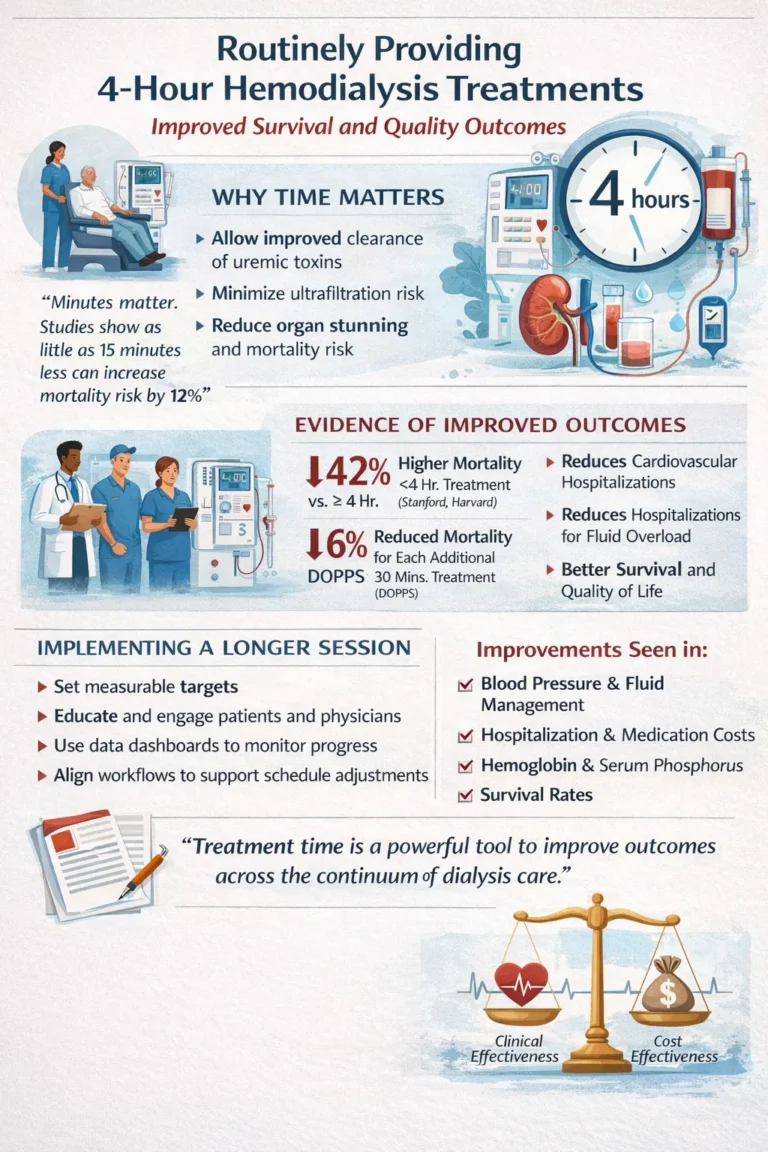
Patients undergoing maintenance hemodialysis continue to experience disproportionately high mortality and substantial treatment-related burden. Among the modifiable aspects of dialysis care, treatment duration represents a potentially powerful yet underused lever to improve outcomes. Accumulating evidence suggests that routinely prescribing 4-hour hemodialysis sessions can meaningfully enhance survival, reduce ultrafiltration-related risk, and improve multiple clinical quality measures.
Despite this evidence, longer treatment times remain inconsistently implemented in routine practice. This article reviews data supporting extended dialysis duration and describes a system-level approach to standardizing 4-hour treatments across a large dialysis organization while accounting for patient preferences, life goals, and perceived care burden.
Rationale for longer treatment duration
The physiologic basis for 4-hour hemodialysis treatments is supported by decades of observational and clinical research. Longer sessions permit more effective clearance of uremic toxins and allow for lower ultrafiltration rates, thereby reducing the risk of intradialytic hypotension and recurrent organ ischemia. Extending treatment time is therefore framed not as a compliance exercise, but as a therapeutic intervention aimed at improving patient-centered outcomes.
Multiple large datasets support this approach. Studies conducted by investigators affiliated with Stanford and Harvard have demonstrated that hemodialysis sessions lasting less than 4 hours are associated with a 42% increase in mortality, even when conventional adequacy targets such as Kt/V are achieved. Data from the Dialysis Outcomes and Practice Patterns Study further indicate that each additional 30 minutes of treatment time is associated with a 6% reduction in mortality, along with lower risks of all-cause hospitalization, cardiovascular hospitalization, and admissions related to fluid overload. Among incident dialysis patients, prescriptions shorter than 4 hours have been associated with a 37% higher risk of death, and each 15-minute reduction below 240 minutes confers an additional 12% increase in mortality risk.
International comparisons further contextualize these findings. Countries such as Japan and Germany routinely prescribe longer dialysis sessions and report superior outcomes, whereas the United States has the highest proportion of patients receiving treatments shorter than 210 minutes. Internal analyses similarly demonstrated that facilities with longer average treatment times consistently performed better across quality indicators, including adequacy, anemia management, hospitalization rates, and mortality.
Organizational implementation and cultural change
Transitioning to routine 4-hour treatments required more than a clinical protocol change; it necessitated a shift in culture. Historically, some U.S. dialysis programs have emphasized higher blood flow rates or larger dialyzers to achieve adequacy targets rather than extending treatment duration. Addressing this required sustained education, stakeholder engagement, and transparency.
Key concerns included scheduling logistics, operational costs, physician acceptance, and patient willingness to remain on dialysis for longer periods. These were addressed through patient-centered educational materials explaining the relationship between treatment time, symptom burden, recovery, and long-term outcomes. Nephrologists were engaged early, with dissemination of evidence and shared best practices rather than top-down mandates, fostering a collective commitment to improved care.
This approach was implemented across facilities operated by U.S. Renal Care and Satellite Healthcare, beginning with a foundational question: how to achieve measurable improvements in patients’ lives using existing therapeutic tools.
Practical strategies for implementation
Clear and measurable targets were established, including prescribing 4-hour treatments for 60% of new patients and 50% of the overall patient population, with appropriate exceptions for palliative care or individualized clinical considerations. Real-time data dashboards were used to track progress, benchmark facilities, and share outcomes across regions.
Facilities in Alaska and Hawaii, which demonstrated longer average treatment times and strong quality outcomes despite geographic constraints, served as exemplars and shared operational strategies with other centers. Clinicians were equipped with patient-facing tools, including videos explaining the effects of longer treatments on hospitalization, mortality, and quality of life. As one facility medical director noted, “Once patients understood the why, acceptance grew dramatically.”
Operational workflows were adjusted to minimize inefficiencies, particularly between treatment shifts. Coordinated, facility-wide scheduling changes—supported by physician leadership—facilitated patient acceptance and streamlined transportation logistics. Several facilities successfully extended treatment times to 4 hours for more than 70% of patients through coordinated implementation.
Progress was recognized at multiple organizational levels, including local leadership acknowledgment, system-wide communications, and direct outreach from senior leadership to facilities achieving meaningful improvements.
Clinical and economic outcomes
Longer dialysis treatments were associated with improvements beyond survival. Clinical studies demonstrated lower blood pressure, improved volume control, higher hemoglobin levels without increased erythropoiesis-stimulating agent use, reduced serum phosphorus, and higher serum albumin. These improvements were accompanied by reductions in hospitalization and medication costs.
Operationally, standardizing treatment duration simplified scheduling for both staff and patients. Over a 12-month period, the proportion of patients prescribed 4-hour treatments increased by 33% overall and by 100% among new patients. Mean treatment duration increased by approximately 15 minutes per session, while labor costs rose by less than $1 per treatment, suggesting favorable cost-effectiveness.
Patient and staff perspectives
Qualitative feedback supported these quantitative findings. Nursing staff reported fewer episodes of intradialytic hypotension and improved patient tolerance. Providers observed fewer missed treatments, with patients reporting better post-dialysis energy levels. One patient remarked, “I was hesitant at first, but now I feel less drained after dialysis.”
These experiences reinforce the principle that treatment time is a critical determinant of patient outcomes and experience. As consistently emphasized, minutes matter.
Conclusions
Optimal dialysis care should not be defined solely by historical adequacy metrics. Treatment duration plays a central role in toxin clearance, hemodynamic stability, and long-term outcomes. Prioritizing 4-hour hemodialysis sessions represents a feasible, evidence-based strategy to improve survival and quality of life. While implementation requires organizational commitment and cultural change, the potential benefits for patients and health systems are substantial.
As this work continues, the focus remains on data-driven improvement, collaboration, and sustained patient engagement to redefine standards for high-quality dialysis care.
For further information, contact Mary Dittrich, MD, FASN, Chief Medical Officer, U.S. Renal Care.