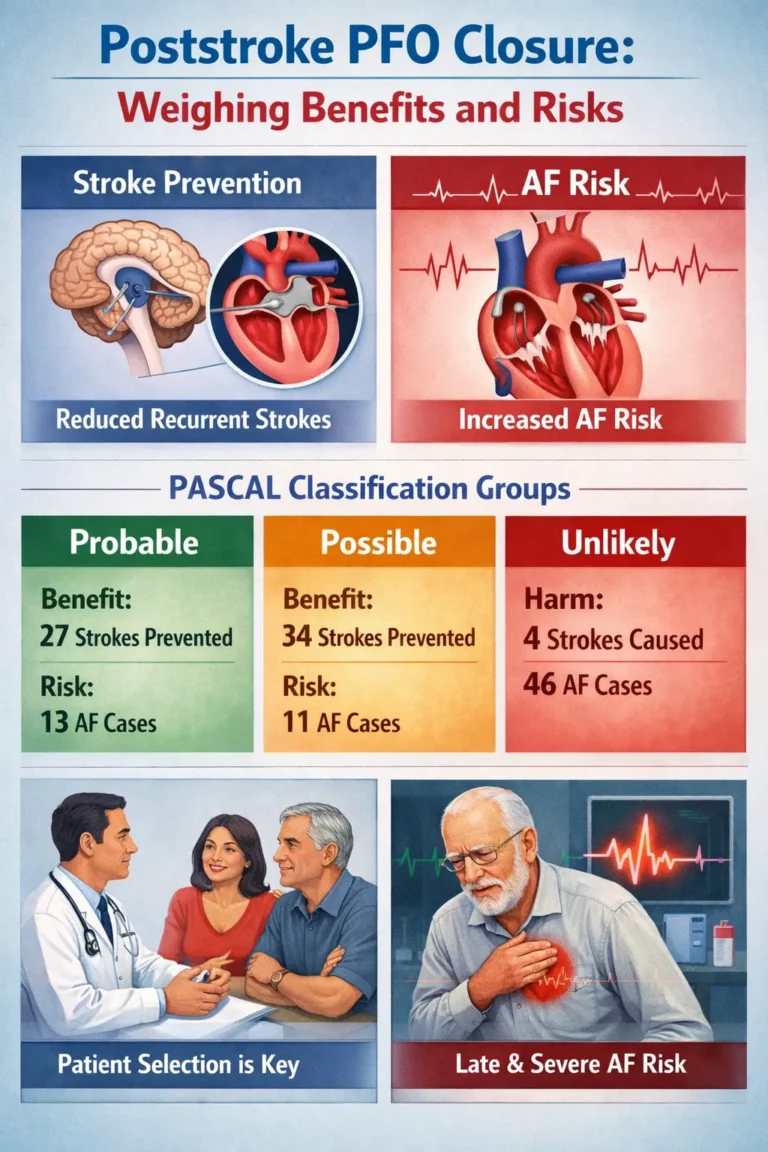
Benefits and Risks of PFO Closure by Causal Likelihood
A recent meta-analysis suggests that the benefits of transcatheter PFO closure for secondary stroke prevention rely heavily on the likelihood that the PFO was the cause of the initial stroke. While the procedure reduces recurrent ischemic stroke in most young and middle-aged adults, it is associated with an increased risk of atrial fibrillation (AF) in a distinct minority of patients.¹
Study Design and Demographics
The study, a secondary analysis of the Systematic, Collaborative, PFO Closure Evaluation (SCOPE) consortium, aggregated individual participant data from six phase 3 randomized clinical trials conducted between 2000 and 2017 across North America, Europe, Australia, Brazil, and South Korea.¹
The analysis included 3740 participants aged 18 to 60 years (mean age, 45 years) presenting with a PFO and a recent cryptogenic ischemic stroke. The demographic breakdown was 55.0% men and 45.0% women. Participants were randomized to either PFO closure plus antithrombotic therapy (n = 1889) or medical therapy alone (n = 1851).¹
The PASCAL Classification System
Outcomes were assessed using the PFO-Associated Stroke Causal Likelihood (PASCAL) system, which categorizes the probability of a stroke being PFO-related as “probable,” “possible,” or “unlikely.” This system integrates the Risk of Paradoxical Embolism (RoPE) score with high-risk echocardiographic markers, such as atrial septal aneurysm and large shunt size.¹
Clinical Outcomes by Group
The analysis evaluated recurrent ischemic stroke (efficacy) and non-periprocedural AF (safety) over a 5-year follow-up period.
1. Probable and Possible Groups (Net Benefit)
Patients classified as having a “probable” or “possible” link between their PFO and stroke demonstrated a reduction in recurrent stroke that outweighed the risk of AF.
-
Probable Group (n = 1382): Closure resulted in a 2.5% absolute reduction in 5-year stroke risk against a 1.3% increase in post-procedural AF. The hazard ratio (HR) for recurrent stroke was 0.10 (P < .001).¹
-
Possible Group (n = 1811): Closure resulted in a 3.4% absolute reduction in stroke risk with a 1.1% increase in late-onset AF. The HR for recurrent stroke was 0.38 (95% CI, 0.22-0.65; P < .001).¹
Jeffrey L. Saver, MD, noted that “PFO closure generally confers net benefit in both probable and possible patients.”¹
2. Unlikely Group (Net Harm)
Conversely, patients classified as “unlikely” to have a PFO-related stroke (n = 547) derived no stroke prevention benefit from the procedure.
-
Stroke Risk: The HR for recurrent stroke was 1.14 (95% CI, 0.53-2.46; P = .74), indicating no statistically significant reduction.¹
-
AF Risk: This group experienced a significant 4.6% absolute increase in late-onset AF (P = .03).¹
Dr. Saver stated, “These findings reinforce that PFO closure should generally be avoided in patients in the unlikely category, among whom [it] causes net harm.”¹
Atrial Fibrillation Characteristics
The study identified 112 AF events, with 83.9% occurring in the closure group. Distinct patterns emerged regarding the timing and severity of AF:
-
In the “probable” and “possible” groups, AF events were clustered within 90 days of the procedure.¹
-
In the “unlikely” group, AF events clustered significantly later, between years 3 and 5. Furthermore, 41.9% of AF events in the unlikely group were classified as severe, compared to only 12.9% in the probable group and 22.0% in the possible group.¹
Projected Clinical Impact per 1000 Patients
The investigators modeled the outcomes over 5 years for every 1000 patients treated:
-
Probable: Closure prevents 27 strokes and causes 13 AF cases.¹
-
Possible: Closure prevents 34 strokes and causes 11 AF cases.¹
-
Unlikely: Closure results in 4 additional strokes and causes 46 additional AF cases.¹
Expert Commentary
David M. Kent, MD, MS, emphasized the utility of the findings for clinical practice, noting that while the relative risk reduction is more modest for the “possible” group than the “probable” group, the absolute benefit is comparable. He stated that the “possible” group’s outcomes are a “marked distinction to the PASCAL unlikely patient, who get no benefit and are subject to increase procedure-related harm.”¹
Matthew I. Tomey, MD, who was not involved in the study, agreed that the results support the use of PASCAL for patient selection. He remarked, “Balanced against the concurrent significant device-related increase in AF, patients for whom attribution of stroke to a PFO is ‘unlikely’ should rarely, if ever, undergo PFO closure for purpose of secondary stroke prevention.”¹
References
-
Borreli L. Poststroke PFO Closure Helps Some, But Not All, Younger Adults. Medscape Medical News. February 02, 2026. Accessed February 11, 2026.