Brief Report: Prevalence and Economic Burden of Chronic Conditions in the Commercially Insured US Population (2024)
Overview
A 2024 analysis conducted by FAIR Health presents new data regarding the epidemiology and economic impact of chronic disease within the United States’ commercially insured population. The report underscores the significant burden of morbidity, revealing that 57.5% of assessed individuals presented with at least one chronic condition. These findings align with broader surveillance data indicating that heart disease remains the leading cause of mortality, further highlighting “the need for greater chronic disease prevention.”
Prevalence and Comorbidity
The cross-sectional analysis of commercial claims data covering 44 chronic conditions indicates a high prevalence of morbidity. In 2024, 57.5% of patients were diagnosed with a single chronic condition, while multimorbidity was common: 11.5% of patients presented with two conditions, and 9.1% with three.
Hyperlipidemia was identified as the most prevalent condition (crude prevalence: 21.2%), followed by hypertension (20.0%), anxiety disorders (14.6%), obesity (13.2%), and mental illness (10.5%).
Significant overlap was observed among metabolic and cardiovascular risk factors. Approximately 33.4% of the cohort presented with obesity, hypertension, hyperlipidemia, or a combination thereof. Notably, 4.3% of patients were diagnosed with all three conditions concurrently. Among patients with one of these diagnoses, 50% exhibited at least one additional comorbidity.
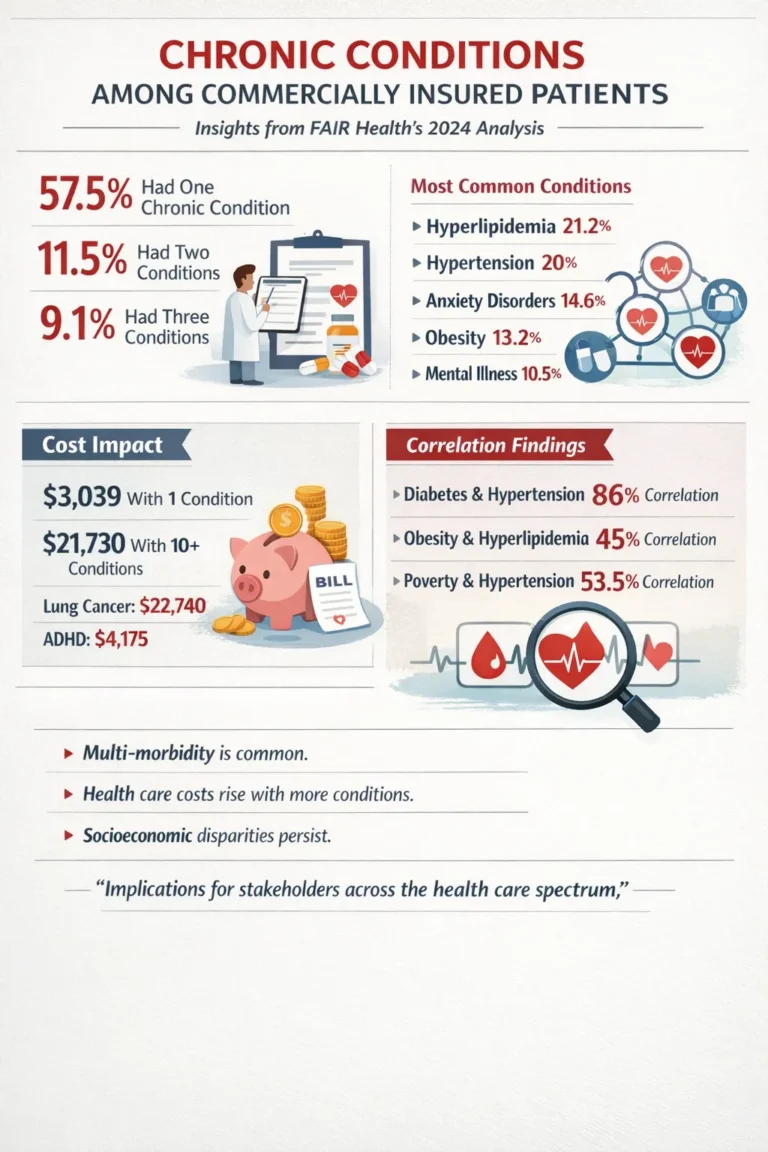
Correlation analysis revealed varying strengths of association between specific dyads:
-
Strongest Positive Correlation: Diabetes and hypertension ($r=0.86$).
-
Weakest Positive Correlation: Obesity and hyperlipidemia ($r=0.45$).
-
Disease Clustering: The median comorbidity burden varied by index condition; patients with non-Alzheimer’s dementia, Alzheimer’s disease, or acute myocardial infarction presented with a median of six comorbidities, whereas those with autism or pneumonia presented with a median of one.
Economic Analysis
The study elucidates a dose-response relationship between chronic disease burden and healthcare expenditures. The average allowed amount—defined as the maximum insurer payment prior to beneficiary cost-sharing—demonstrated marked stratification:
-
Zero Chronic Conditions: $1,590.
-
One Chronic Condition: $3,039 (approximately a two-fold increase).
-
$ge$10 Chronic Conditions: $21,730 (a 13.7-fold increase relative to the zero-condition cohort).
Variance in cost was also observed across specific pathologies. Lung cancer was associated with the highest mean annual allowed amount ($22,740), while attention-deficit/hyperactivity disorder (ADHD) was associated with the lowest ($4,175).
Socioeconomic Determinants
The analysis identified specific correlations between poverty rates and disease prevalence. A moderate positive correlation (53.5%) was observed between the poverty rate and hypertension prevalence. Furthermore, a specific phenotype cluster—comprising obesity, hypertension, diabetes, chronic kidney disease, and hyperlipidemia—demonstrated a strong correlation with higher poverty rates. Conversely, oncology diagnoses generally showed weak correlations with poverty, with breast cancer exhibiting an inverse relationship (correlation: –24.3%).
Limitations and Implications
The authors note that this observational analysis has not undergone peer review and is limited by the exclusion of Medicare Advantage and Medicare Parts A, B, and D beneficiaries. Despite these limitations, FAIR Health asserts that the data

“have implications for stakeholders across the health care spectrum, including patients, providers, payors, policymakers and researchers.”