[ad_ 1]
A New Kind of Tumor Board: Tackling Cancer Pain Head-On.
A pioneering multidisciplinary tumor board has been established with a singular focus — managing cancer-related pain, particularly that arising from bone metastases. This initiative aims to enhance patients’ quality of life, minimize opioid dependence, and ensure cancer treatment proceeds without interruption.
Tumor boards traditionally play a critical role in collaborative cancer care, helping clinicians exchange insights and refine treatment strategies. However, for Dr. Alan Alper Sag, associate professor of interventional radiology at the University of Miami Miller School of Medicine, a simple yet profound question reshaped that model:
“What if the disease was pain?”
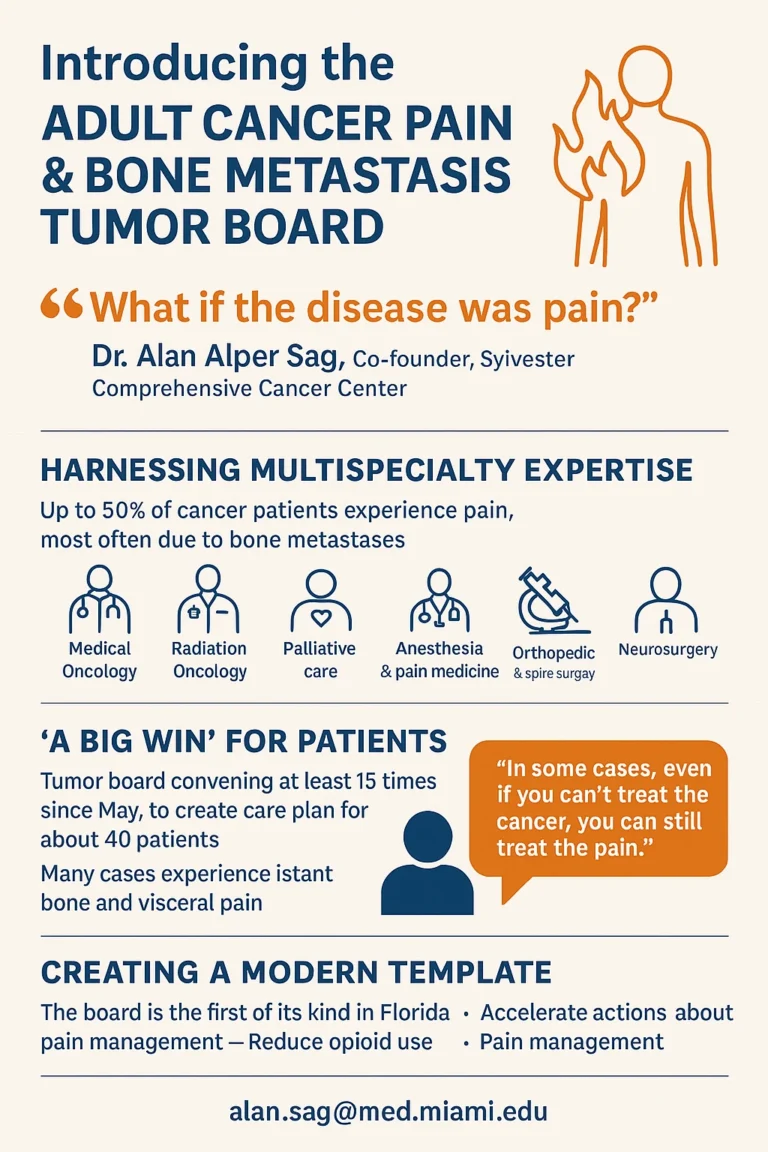
He wondered if specialists could unite not only to treat cancer itself but also to directly confront the pain that often comes with it. The result of that idea is the Adult Cancer Pain & Bone Metastasis Tumor Board at Sylvester Comprehensive Cancer Center, a first-of-its-kind effort in Florida and among only a few in the United States.
Reframing Cancer Pain Management
Dr. Sag and his colleagues developed the board to focus specifically on patients whose pain is complex or undertreated in conventional tumor discussions. The objective, he explains, is to manage pain “as aggressively, strategically, and effectively as we treat the cancer itself.”
Pain is a common issue — up to 50% of patients receiving active cancer therapy experience it at varying levels. With improvements in survival, pain has become even more prominent, particularly from bone metastases, the leading source of cancer-related discomfort. Unfortunately, once patients reach maximum allowable doses of radiation or chemotherapy, therapeutic options dwindle.
Opioids often become the fallback, but their side effects — including sedation, constipation, nausea, mood changes, and cognitive issues — can severely impact life quality.
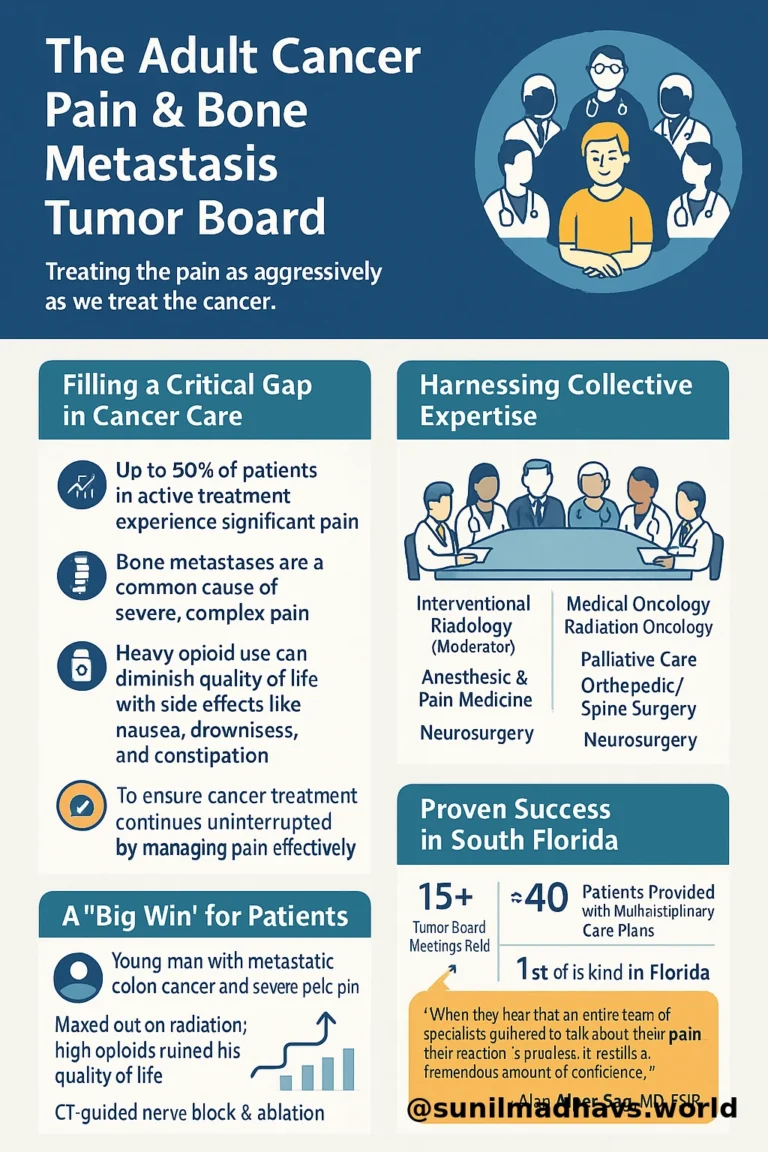
The new tumor board seeks to accelerate decision-making in pain management by integrating expertise from various specialties. The team’s collaborative care plans emphasize multimodal, opioid-sparing strategies that align with National Comprehensive Cancer Network (NCCN) guidelines.
A Multispecialty Effort
Each meeting is led by an interventional radiologist and includes professionals from:
Medical and radiation oncology
Palliative care
Anesthesia and pain medicine
Orthopedic and spine surgery
Neurosurgery
The members collectively review patient histories, imaging, and previous interventions before discussing tailored pain-relief options. The conversation often explores questions like:
Is the patient a candidate for surgery or additional radiation?
Would multimodal analgesia help?
Can nerve blocks, ablations, or neuromodulation techniques be used?
This model ensures that no potential avenue for relief is overlooked and that every perspective contributes to improving the patient’s comfort and functionality.
Real-World Impact
Since launching in May, the board has convened around 15 times, creating detailed, multidisciplinary care plans for roughly 40 patients — most suffering from bone or visceral pain.
One notable case involved a patient with head and neck cancer whose pain required coordinated input from multiple surgical and oncology subspecialties. Another involved a young man with metastatic colon cancer and severe pelvic pain unrelieved by radiation or opioids. After discussion, the team opted for a CT-guided nerve block and ablation, which provided immediate, complete pain relief.
As Dr. Sag explained, “When pain suddenly disappears, some patients are so surprised they don’t know how to respond — they’ve been suffering for so long.”
Building a New Model for Care
The Adult Cancer Pain & Bone Metastasis Tumor Board represents a novel, forward-thinking framework for addressing pain in cancer care. It complements existing tumor boards by broadening participation and deepening focus. Only a few similar boards exist nationally — notably at Brown University and Emory University — but the Miami model may soon serve as a template for other institutions.
Case referrals are open across the University of Miami Health System and Jackson Health System, ensuring that any clinician can submit patients for discussion.
Feedback from oncologists and advanced practice providers has been overwhelmingly positive. Many note that the board’s work has:
Reduced hospital admissions related to pain crises.
Improved outpatient pain control
Decreased reliance on opioids
Enhanced overall patient experience
Patients themselves express deep gratitude, often saying it’s reassuring to know that “an entire team of specialists met specifically to discuss their pain.”
A “Winning Strategy” for Institutions Nationwide
Dr. Sag continues to engage with specialists at national meetings to compare approaches and share lessons from Sylvester’s experience. He encourages other medical centers interested in forming similar boards to start with an internal discussion of unmet needs, referencing the NCCN adult cancer pain guidelines to identify key specialties to include.
“Start with a core group of motivated, capable people who share the mission,” he advises.
Contact Information
For more details, clinicians can reach out to:
Alan Alper Sag, MD, FSIR
Email: alan.sag@med.miami.edu
In essence:
This initiative reframes how cancer care teams think about pain — not as a secondary issue, but as a disease state deserving the same attention, collaboration, and innovation as cancer itself.