Serum Vitamin D Status and Risk of Respiratory Tract Infection–Related Hospitalization
**Bournot AR, et al.** *American Journal of Clinical Nutrition.* 2025; doi:10.1016/j.ajcnut.2025.101179.
—
## Background
Vitamin D plays a critical role in musculoskeletal health and immune function. Increasing evidence suggests that its antibacterial and antiviral properties may influence susceptibility to respiratory tract infections (RTIs), which remain a major cause of hospitalization worldwide. Despite biologic plausibility, robust population-level data linking vitamin D status to RTI-related hospitalizations have been limited.
Abigail R. Bournot, MSc, ANutr, emphasized the physiologic importance of the nutrient, stating,
> “Vitamin D is vital to our physical well-being. Not only does it keep our bones and muscles healthy, its antibacterial and antiviral properties are also thought to help reduce the risk of respiratory tract infections that can lead to hospitalization.”
She further noted,
> “This research attaches hard data to support the theory.”
—
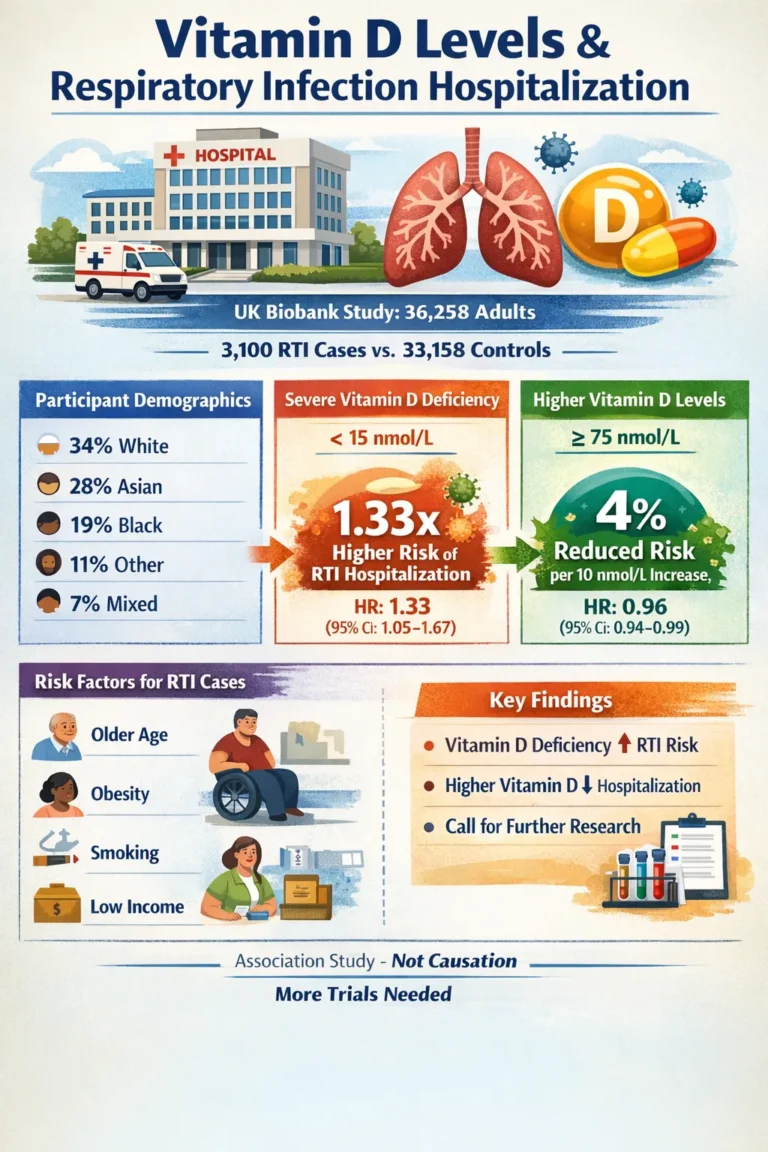
## Study Design and Population
Investigators conducted an unmatched case–control analysis using data from the UK Biobank to evaluate whether serum 25-hydroxyvitamin D (25[OH]D) concentrations were associated with hospitalization for respiratory tract infections.
The study included **36,258 adults** representing diverse racial and ethnic backgrounds:
* 34% White
* 28% Asian
* 19% Black
* 11% Other
* 7% Mixed ethnicity
Among these participants, **3,100 adults (8.5%) experienced at least one RTI**, whereas **33,158 adults did not**.
—
## Baseline Characteristics
Participants hospitalized for RTIs differed from those who were not across several clinical and sociodemographic variables:
* **Male sex:** 53% vs. 45.7%
* **Age >60 years:** 44.9% vs. 25.6%
* **BMI ≥30 kg/m²:** 41% vs. 28.9%
* **Severe vitamin D deficiency (<15 nmol/L):** 13.7% vs. 10.6%
* **Income <£18,000:** 43.2% vs. 27.1%
* **Self-reported fair/poor health:** 52.8% vs. 30.9%
* **Current smoking:** 15% vs. 11%
* **Statin use:** 34.8% vs. 18.1%
These differences highlight the multifactorial risk profile associated with RTI-related hospitalization.
—
## Primary Findings
Using a Cox proportional-hazards model, investigators observed a significant inverse relationship between serum vitamin D levels and RTI hospitalization risk.
For every **10 nmol/L increase in serum 25(OH)D**, the risk of hospitalization declined by approximately **4%**:
* **Hazard ratio (HR): 0.96**
* **95% CI: 0.94–0.99**
Consistent with this trend, adults with severe deficiency experienced substantially higher risk compared with those who had sufficient vitamin D levels (≥75 nmol/L):
* **HR: 1.33**
* **95% CI: 1.05–1.67**
By contrast, no statistically significant differences were identified between individuals with sufficient levels and those whose concentrations ranged from **15 to 74 nmol/L**. Binary logistic regression analyses produced similar patterns, reinforcing the robustness of the association.
## Interpretation and Public Health Implications
Andrea L. Darling, PhD, highlighted the broader implications of these findings:
> “Our findings of a significant association between increased vitamin D levels in our bodies and reduced hospital admission rates warrants further study, and points to the potential for vitamin D supplementation and consumption of vitamin D fortified foods to reduce the risk of hospitalization with respiratory infections in the future, and therefore mitigate pressures on the NHS.”
Collectively, the results suggest that severe vitamin D deficiency may represent a modifiable risk factor for RTI-related hospitalization, with potential implications for preventive strategies and health system burden.
—
## Perspective
Kathleen Garcia-Benson, RDN, CSSD, CPT, described the results as largely expected yet clinically meaningful, noting that they may support preventive care initiatives aimed at reducing both illness burden and health care expenditures.
She observed that the study’s scale was notable, particularly the linkage of vitamin D measurements with hospitalization records for more than 35,000 participants. However, she cautioned that some deficient individuals may not have been captured if they did not develop infections. Accordingly, the data demonstrate correlation rather than causation but nonetheless underscore an important relationship warranting further investigation.
Garcia-Benson emphasized vitamin D’s broad physiologic relevance, explaining that it is commonly recommended for individuals with limited sun exposure or reduced cutaneous synthesis. Beyond bone health, the nutrient contributes to sustained energy, immune competence, brain health, and mental well-being.
In clinical practice, vitamin D deficiency is frequently encountered. The findings therefore support routine screening during annual wellness and chronic-care visits, followed by supplementation when appropriate and supported by insurance coverage.
She also noted persistent uncertainty regarding optimal serum ranges:
> “As a health care provider, it would be helpful to have clearer guidance on who would benefit from maintaining a level closer to 30 ng/mol vs. 70 ng/mol, since in health, more is not always better, and the current range is broad.”
Garcia-Benson added that clinicians could enhance care not only through supplementation but also by referring patients to registered dietitians who can promote consistent intake of vitamin D–rich foods alongside broader preventive health strategies.
—
## Limitations
Although the large dataset strengthens the analysis, the observational design precludes causal inference. Residual confounding may remain, and the absence of infection among some deficient individuals could influence risk estimates.
Further randomized studies are needed to clarify whether vitamin D supplementation directly reduces RTI hospitalizations and to define optimal therapeutic thresholds.
—
## Conclusion
In a large UK Biobank cohort, higher serum 25-hydroxyvitamin D concentrations were associated with a significantly lower risk of hospitalization for respiratory tract infections, whereas severe deficiency conferred increased risk. These findings support continued investigation into vitamin D as a potentially modifiable factor in respiratory illness prevention while
underscoring the need for randomized clinical trials to establish causality and refine target serum levels.