:
Over Half of Adults with IBD Have At Least One Mental Health Condition, Study Finds
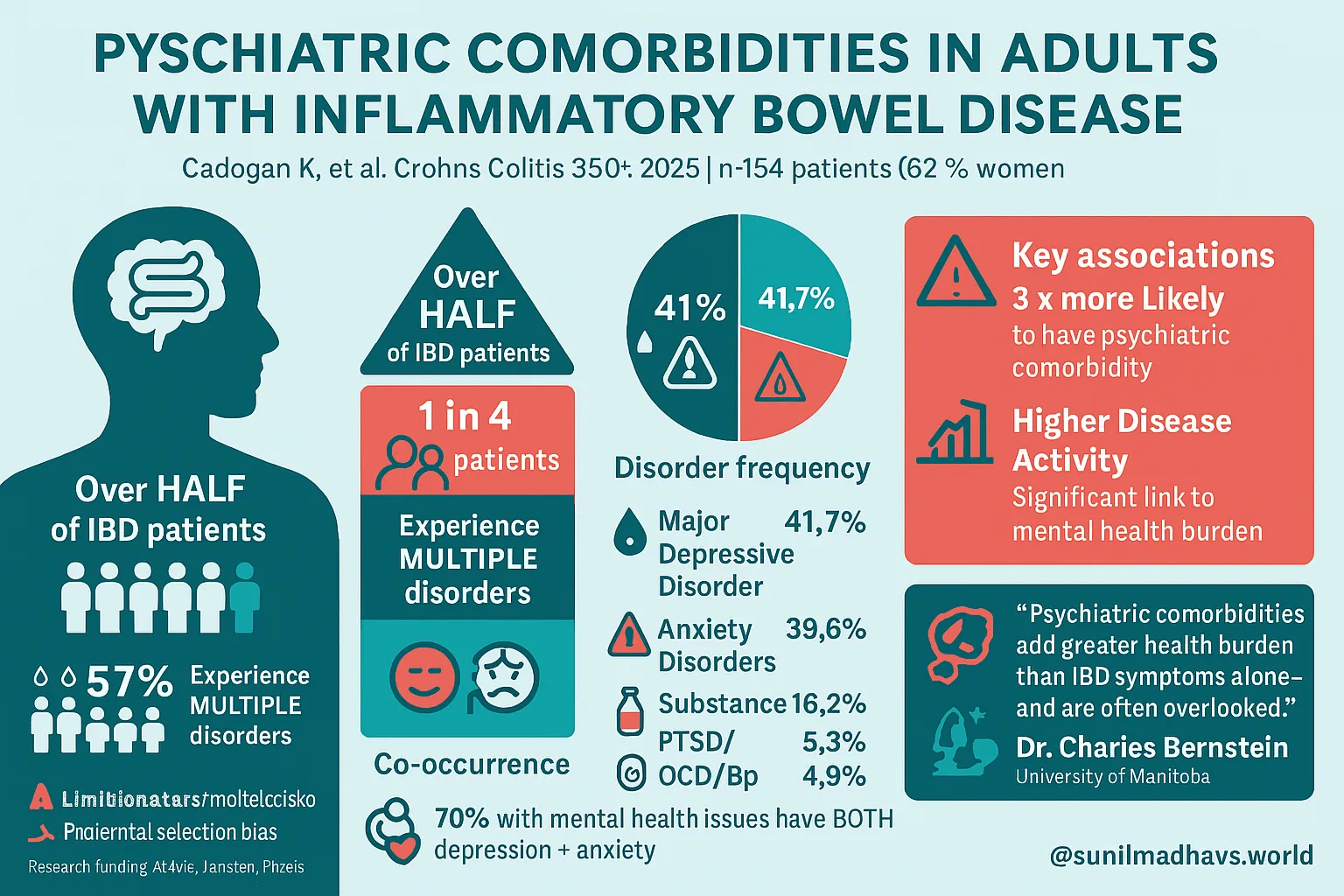
A recent study published in Crohn’s & Colitis 360 revealed that more than 50% of adults living with inflammatory bowel disease (IBD) also have at least one psychiatric comorbidity. Additionally, around 27% of patients were diagnosed with multiple psychiatric disorders, indicating a substantial mental health burden in this population.
Why This Matters
The findings underscore the critical need for integrated care that addresses both mental and physical health in individuals with IBD. According to Dr. Charles N. Bernstein, MD, FRCPC — the study’s lead author and a distinguished professor at the Max Rady College of Medicine — psychiatric issues can significantly impact a patient’s overall health and quality of life, sometimes even more than the gastrointestinal symptoms themselves.
“This study shows how common psychiatric conditions are among IBD patients,” said Bernstein. “Multiple comorbidities can significantly worsen the overall health burden.”
Background and Study Design
Historically, psychiatric research in IBD patients has primarily focused on depression and anxiety, but little attention has been paid to other psychiatric disorders. Bernstein and his research team conducted a cross-sectional analysis using data from a 3-year prospective longitudinal study examining psychiatric disorders in individuals with immune-mediated inflammatory diseases, including IBD, multiple sclerosis, and rheumatoid arthritis.
For this specific analysis, the researchers looked exclusively at 154 adult participants diagnosed with IBD, 62% of whom were women and 63% diagnosed with Crohn’s disease.
Data Collection and Evaluation
- Participants reported their smoking status, physical health conditions, and other baseline characteristics.
- Trained professionals conducted structured psychiatric interviews using the DSM-IV criteria, supplemented with PTSD assessments using DSM-5 standards.
- IBD disease activity was measured using:
- The Powell Tuck Index for Ulcerative Colitis.
- The Harvey Bradshaw Index for Crohn’s Disease.
Key Findings
- 57% of patients had at least one psychiatric comorbidity.
- 27% had more than one mental health diagnosis.
- The most prevalent psychiatric conditions included:
- Major Depressive Disorder – 41.7%
- Anxiety Disorders – 39.6%
- Substance Use Disorders – 16.2%
- PTSD – 5.3%
- Obsessive-Compulsive Disorder (OCD) – 4.9%
- Bipolar Disorder – 2%
Combinations of disorders were common:
- Nearly half (49.1%) of those with both major depressive disorder and another condition also had a substance use disorder.
- Among individuals with at least one psychiatric diagnosis, over 70% had both depression and anxiety.
Clinical Implications
Dr. Bernstein emphasized the importance of gastroenterologists screening IBD patients for mental health concerns. “While depression and anxiety are most frequently observed, we must recognize the presence of other psychiatric disorders like substance use issues,” he said.
He called for mental health resources to be made available for individuals with IBD, noting that mental illness adds a significant burden to the existing challenges of managing chronic gastrointestinal conditions.
Associated Risk Factors
The analysis revealed significant associations:
- Current smokers were more likely to have a psychiatric comorbidity (P < .001).
- Patients with higher IBD activity scores also had increased psychiatric burden (P = .005).
Study Limitations and Future Directions
While the study provides crucial insights, the authors acknowledged some limitations:
- It does not establish a clear timeline between the onset of psychiatric disorders and IBD progression.
- There may be selection bias, as participants were aware the study focused on mental health, which could affect who chose to participate.
Dr. Bernstein noted the importance of long-term research: “We need to follow a large cohort of IBD patients over time to understand how mental health conditions evolve after IBD diagnosis.”
Contact and Disclosures
Contact: Dr. Charles N. Bernstein – charles.bernstein@umanitoba.ca
- Disclosures: Dr. Bernstein has financial ties with several pharmaceutical companies including AbbVie, Amgen, Janssen, Pfizer, Takeda, and others in various capacities (advisory roles, research funding, speaker panels, and educational grants). Please refer to the study for the full list of disclosures for all authors.
Let me know if you’d like this turned into a graphic, plain-text summary, or social media post.