- Key Highlights:
-
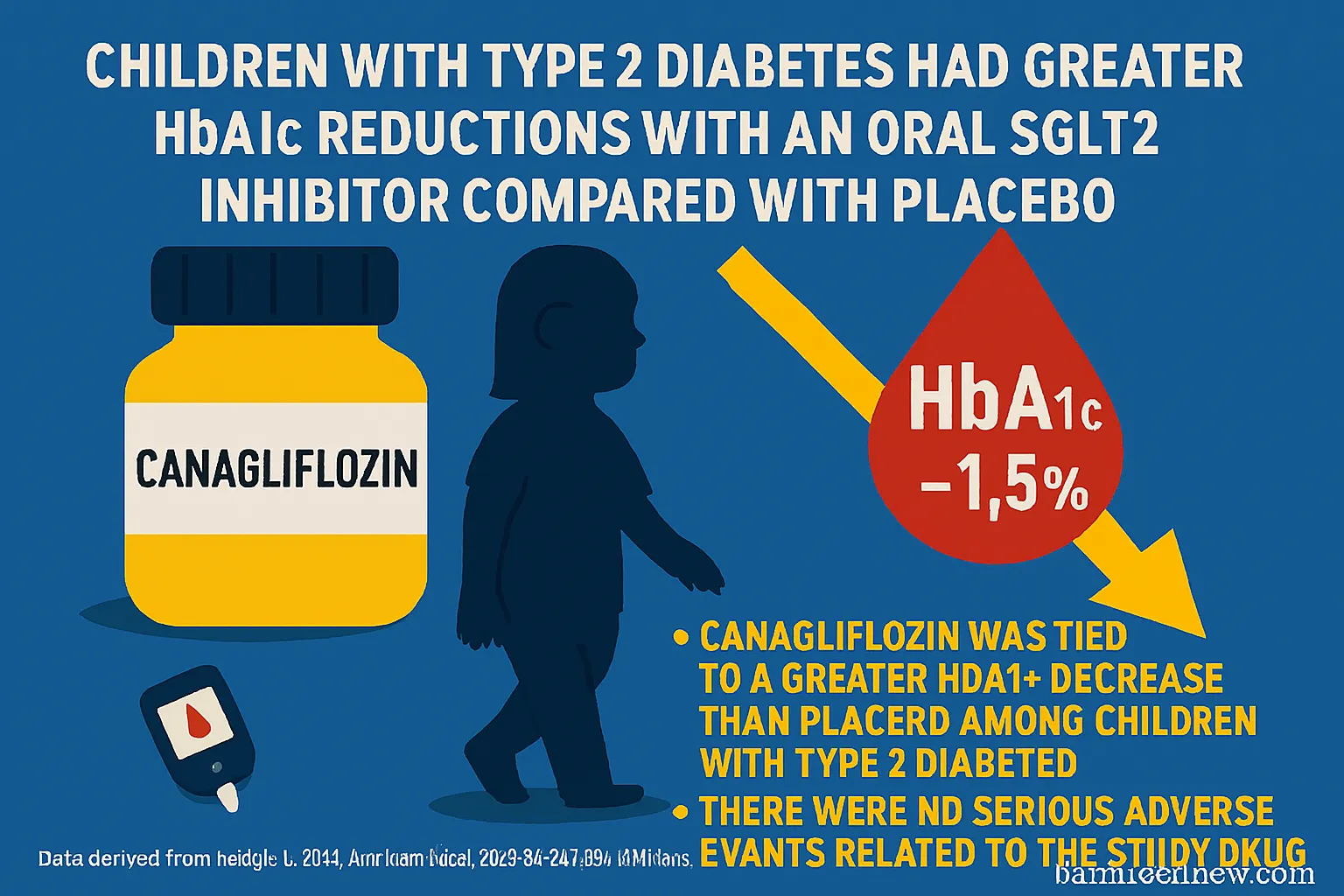
Canagliflozin significantly reduced HbA1c levels compared to placebo in children and adolescents with type 2 diabetes.
-
The drug showed a good safety profile, with no serious side effects attributed to it.
Study Overview & FDA Approval
Children and teens with type 2 diabetes showed a greater reduction in blood sugar (HbA1c) when treated with the oral SGLT2 inhibitor canagliflozin (Invokana, Janssen) than those receiving a placebo.
This finding supported the FDA’s decision in December 2024 to expand the drug’s approved use to include individuals aged 10 to 17 years. The approval was based on results from a phase 3 randomized controlled trial, recently published in the Annals of Internal Medicine.
Trial Details
-
Participants: 171 youths (aged 10–17) with HbA1c between 6.5% and 11%, who had already been on a diet and exercise program for at least four weeks, with or without metformin.
-
Design: After a 2-week preparation period, participants were randomly assigned to receive 100 mg canagliflozin (n = 84) or placebo (n = 87) once daily.
-
At week 13, participants still above target HbA1c levels could either:
-
Continue 100 mg, or
-
Increase to 300 mg of canagliflozin.
-
-
Duration: The study continued for one year.
-
Main goals: Evaluate Hb
 A1c changes and drug safety over 26 weeks.
A1c changes and drug safety over 26 weeks.
Results: Blood Sugar Control
-
At 26 weeks, the canagliflozin group had a mean HbA1c reduction of –0.76 percentage points vs. placebo (P = .002).
-
Among those also on metformin, results were similar (–0.77 percentage points, P = .012).
-
Canagliflozin also led to a larger drop in fasting plasma glucose at:
-
26 weeks: –25.5 mg/dL
-
52 weeks: –27.8 mg/dL
-
Proportion of Patients Meeting HbA1c Targets:
-
At 26 weeks:
-
HbA1c <6.5%: 36.3% (canagliflozin) vs. 14% (placebo)
-
HbA1c <7%: 45.7% vs. 32.8%
-
-
At 1 year:
-
HbA1c <6.5%: 30.9% vs. 15.6%
-
HbA1c <7%: 47.2% vs. 28.9%
-
-
Rescue medication was required by:
-
46% of the placebo group
-
Only 11.9% of the canagliflozin group
-
-
Body weight also declined more in the canagliflozin group (by 1.6 percentage points)
Safety Profile
-
Adverse events: Reported in 77.4% (canagliflozin) vs. 74.7% (placebo).
-
More common side effects with canagliflozin:
-
Headache (10.7%)
-
Nasopharyngitis (9.5%)
-
UTIs (7.1%)
-
Vomiting (6%)
-
-
-
Serious adverse events:
-
Canagliflozin: 9.5%
-
Placebo: 5.7%
-
Specific cases in canagliflozin group: One each of diabetic ketoacidosis, pancreatitis, and fracture (none attributed to the drug).
-
-
Hypoglycemia (low blood sugar):
-
Symptomatic: 11.9% (canagliflozin) vs. 10.3% (placebo)
-
Glucose <70 mg/dL: 17.9% vs. 16.1%
-
Glucose <56 mg/dL: Similar between groups
-
Severe case: Only one, in placebo group
-
Clinical Perspective: A Step Forward
Experts Ryan P. Brady, MD and Amy S. Shah, MD from Cincinnati Children’s Hospital highlighted the trial as a meaningful development in managing youth-onset type 2 diabetes, a condition known to be more aggressive and challenging to manage than in adults.
-
Canagliflozin’s effect on HbA1c lowering is comparable to that of GLP-1 receptor agonists.
-
The editorial emphasized the need for combination therapy, given the high failure rate of single-agent treatments in youths.
-
Brady noted that further research is needed to assess long-term impacts on cardiorenal health and disease progression in young populations.
Conclusion
Canagliflozin offers a safe and effective option for improving blood glucose control in children and adolescents with type 2 diabetes. Its ability to deliver sustained HbA1c reduction, possibly reduce body weight, and delay the need for additional medications makes it a valuable addition to pediatric diabetes