Researchers Develop Automated VEST Algorithm to Improve Pulmonary Arterial Hypertension Detection
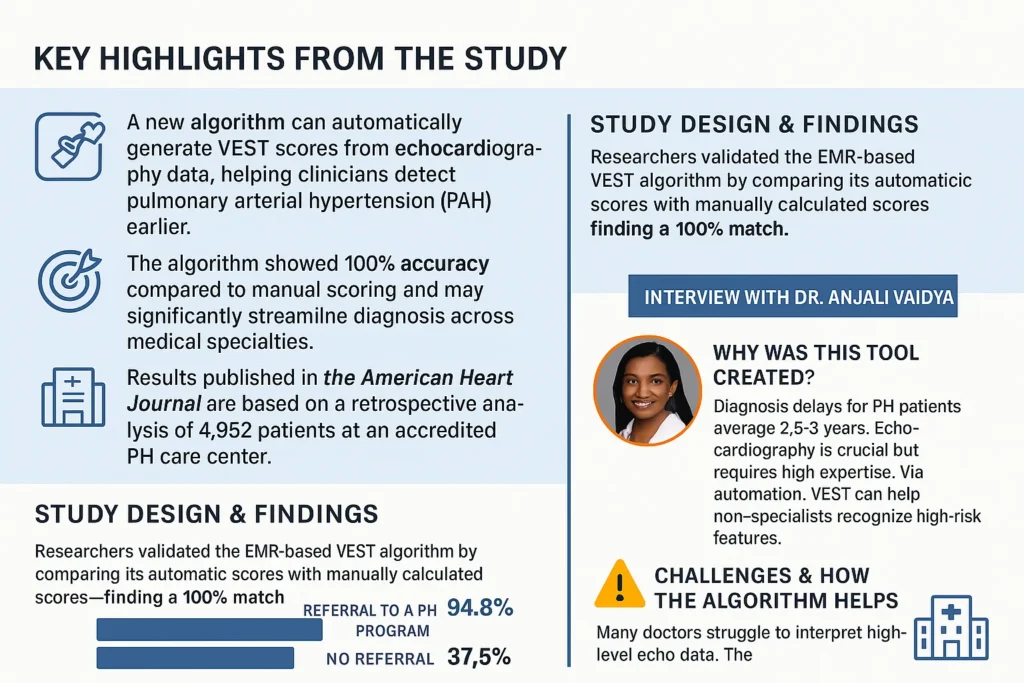
A new study has introduced an automated algorithm designed to calculate a patient’s Virtual Echocardiography Screening Tool (VEST) score, streamlining the process for clinicians and aiding earlier detection of pulmonary arterial hypertension (PAH). This advancement, published in the American Heart Journal, demonstrated that the algorithm’s automatically calculated scores were identical to those derived manually, suggesting strong reliability for widespread clinical use.
The analysis reviewed data from 4,952 adults who had undergone transthoracic echocardiograms at a hospital affiliated with a Cardiology-based Pulmonary Hypertension Center of Comprehensive Care. For patients who scored +3 on the VEST (n=354), researchers found that those referred to a pulmonary hypertension (PH) program were far more likely to undergo gold-standard diagnostic testing with right heart catheterization (94.8% vs. 37.5%) than those not referred.
Addressing Diagnostic Delays and Skill Gaps
Lead author Dr. Anjali Vaidya, Director of the Advanced Pulmonary Hypertension Program at Temple University Hospital, highlighted the motivation behind the research. She explained that PAH patients often face an average diagnostic delay of 2.5 to 3 years from symptom onset. By the time they receive a diagnosis, many can barely walk across a room due to severe shortness of breath.
Echocardiography, central to diagnosing and managing PH, requires significant expertise, often posing a challenge for non-specialists. The study’s goal was to create a simplified, broadly accessible screening tool so that healthcare providers — including primary care physicians, hospitalists, pulmonologists, and non-specialist cardiologists — could identify high-risk patients sooner, without needing advanced echocardiography training.
How the VEST Tool Works
The VEST tool uses standard parameters from echocardiograms, routinely included in reports, to evaluate whether pulmonary hypertension is likely caused by left heart failure or stems from pulmonary arteries leading to right heart failure. Since all PH is a form of heart failure, this distinction is crucial for appropriate referral and management.
Traditionally, calculating the VEST score manually required memorization and time, creating room for error. The automated electronic medical record (EMR)-based algorithm eliminates these hurdles by calculating scores instantly, allowing physicians to assess thousands of patients rapidly and consistently.
Key Findings and Clinical Impact
The study confirmed that the automated VEST algorithm was 100% accurate compared to manual calculations, enabling faster, error-free assessments. Importantly, patients with high scores referred to Temple’s accredited PH center were significantly more likely to receive guideline-based care, including right heart catheterization, compared to those not referred (95% vs. 37%).
Dr. Vaidya noted that this tool could empower clinicians across specialties to identify high-risk PAH patients earlier, ensuring timely referrals to accredited centers and helping meet gold-standard care guidelines. Even experienced PH specialists can benefit from using the tool to prioritize urgent cases when complete imaging or testing is unavailable.
Next Steps
Following the study’s success, researchers are planning collaborations with major health systems in the U.S. and abroad to expand the algorithm’s application in both research and clinical practice. The ultimate goal is to maximize its reach and help detect and treat PAH earlier on a global scale.
For additional information, Dr. Anjali Vaidya can be contacted at anjali.vaidya@tuhs.temple.edu.