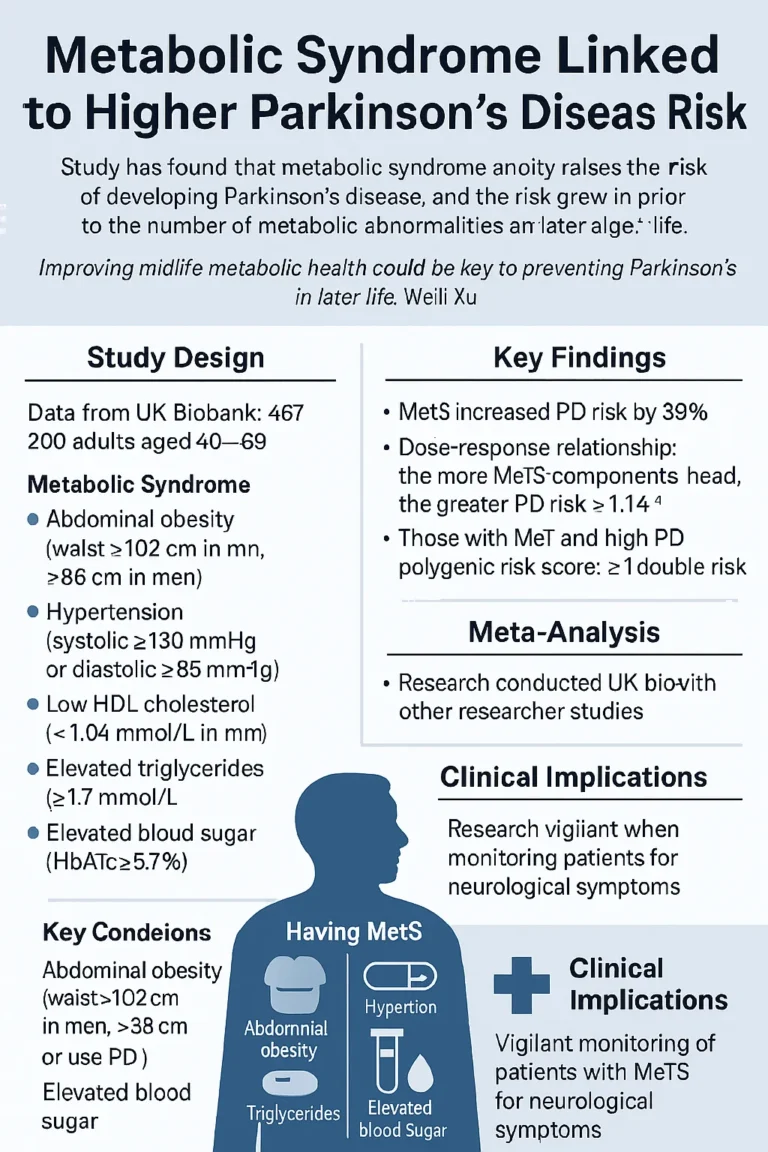
A new study has found that metabolic syndrome (MetS) significantly raises the risk of developing Parkinson’s disease (PD). People with metabolic syndrome were more likely to develop PD compared with those without it, and the risk grew in proportion to the number of metabolic abnormalities present. The findings, published in Neurology, highlight the importance of metabolic health in reducing neurological risks.
According to lead researcher Weili Xu, PhD, professor of neurobiology, care sciences and society at the Karolinska Institute in Sweden, improving midlife metabolic health could be a key preventive measure against Parkinson’s in later life.
Study Design and Population
The investigation used data from the UK Biobank, focusing on adults aged 40 to 69 who lived within 40 kilometers of one of 23 UK assessment centers. A total of 467,200 participants were included, with an average age of 56.5 years, and slightly more than half (54.3%) were women. Of these, 177,407 participants (38%) had MetS.
Metabolic syndrome was defined as having three or more of the following five conditions:
- Abdominal obesity (waist >102 cm in men, >88 cm in women)
- Hypertension (systolic ≥130 mmHg, diastolic ≥85 mmHg, or use of antihypertensives)
- Low HDL cholesterol (<1.04 mmol/L for men, <1.3 mmol/L for women, or taking lipid-lowering drugs)
- Elevated triglycerides (≥1.7 mmol/L or treated with lipid-lowering drugs)
- Elevated blood sugar (HbA1c ≥5.7%)
Researchers also calculated a polygenic risk score (PRS-PD) for each participant, based on 26 PD-associated genetic variants, and classified individuals into low, moderate, or high genetic risk categories.
Participants were tracked for a median of 15 years, during which 3,222 individuals developed PD.
Key Findings
- Having MetS increased the risk of PD by 39% compared with participants without MetS (HR = 1.39; 95% CI: 1.11–1.74).
- A dose-response relationship was observed: the more MetS components a person had, the greater their PD risk (HR per component = 1.14; 95% CI: 1.05–1.24).
- Risk was especially elevated among individuals who had both MetS and a high PD polygenic risk score, with more than double the risk (HR = 2.58; 95% CI: 2.12–3.14).
- Specific metabolic components also contributed to elevated PD risk:
- Central obesity → 33% higher risk
- Obesity (general) → 43% higher risk
- Low HDL cholesterol → 28% higher risk
- High blood sugar → significantly elevated risk
The study also found that participants with MetS were more likely to be older, male, white, and have higher socioeconomic status than those without MetS. Incidence rates showed a difference: 4.87 cases per 10,000 person-years in those without MetS vs. 5.21 cases in those with MetS.
Meta-Analysis
To strengthen their findings, the researchers conducted a meta-analysis by pooling UK Biobank data with eight other observational studies. Reviewing 24.7 million participants and 98,582 PD cases, they found that MetS was associated with a 29% higher PD risk (HR = 1.29; 95% CI: 1.15–1.44). The association was consistent across all five MetS components.
Clinical Implications
The study suggests that clinicians should be more vigilant in monitoring patients with metabolic syndrome, particularly those with genetic predisposition to PD. Early recognition of neurological symptoms in these individuals could lead to improved outcomes.
Dr. Xu emphasized a positive takeaway:
“The same lifestyle choices that protect against heart disease and diabetes may also help protect against neurodegenerative diseases like Parkinson’s,” Xu noted.
Funding and Disclosures
The research was supported by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, the Karolinska Institute Research Foundation, and Lindhes Avokatbyra AB. Full author disclosures are available in the original publication.