New Framework Could Redefine Obesity for Nearly 1 in 5 U.S. Adults
A recent cross-sectional and longitudinal analysis, published in the Annals of Internal Medicine, indicates that adopting a new European Association for the Study of Obesity (EASO) framework for diagnosing and managing obesity could significantly shift how Americans are classified. Under this system, 18.8% of U.S. adults who were previously labeled as “overweight” by BMI standards would now be considered as having obesity.
What’s New About the EASO Framework?
Traditional obesity classification relies heavily on BMI alone, which has long been criticized for not capturing other risk factors like fat distribution and related health issues. The EASO model takes a multifactorial approach, defining obesity as:
-
BMI ≥ 30 kg/m², or
-
BMI 25–<30 kg/m² combined with a waist-to-height ratio ≥ 0.5, plus the presence of functional, medical, or psychological complications.
This approach aims to better identify individuals at health risk who might have been overlooked by BMI-only measures. Dr. Dror Dicker, associate professor of internal medicine at Tel Aviv University and lead author, noted that this broader definition has major implications: millions of people will now require clinical attention and tailored care, which will force policy changes and health care systems to adapt services for these newly classified individuals.
Study Findings
Researchers analyzed NHANES (National Health and Nutrition Examination Survey) data from 1999–2018, covering 44,030 Americans aged 18–79 years. They found:
-
18.8% of adults who were classified as overweight under BMI-only standards now meet the criteria for obesity.
-
Common health issues among this newly reclassified group included:
-
Hypertension (79.9%)
-
Arthritis (33.2%)
-
Diabetes (15.6%)
-
Cardiovascular disease (10.5%)
-
In terms of mortality risk:
-
These individuals did not show a significantly greater risk of death than those with normal weight who also had comorbidities.
-
Compared to healthy-weight individuals with no major health issues, they had a 50% higher mortality risk (HR = 1.5; 95% CI, 1.2–1.88).
-
This risk, however, was similar to that of normal-weight individuals with comorbidities (HR = 1.74; 95% CI, 1.34–2.22). Me
-
People with a BMI ≥ 30 kg/m² (traditional obesity definition) still showed the highest mortality risk overall (HR = 1.19; 95% CI, 1.08–1.32).
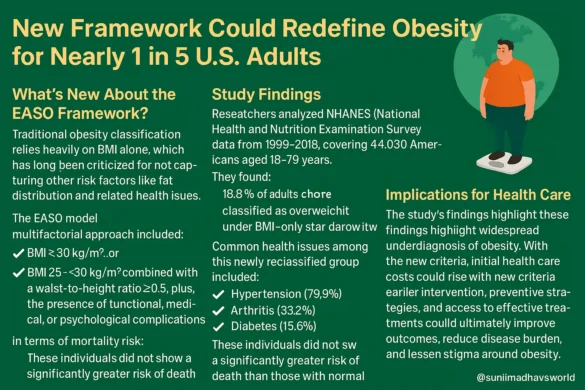
Implications for Health Care
The study’s authors suggest that these findings highlight widespread underdiagnosis of obesity. With the new criteria, initial health care costs could rise as more people qualify for obesity care. However, earlier intervention, preventive strategies, and access to effective treatments could ultimately improve outcomes, reduce disease burden, and lessen stigma around obesity.
They emphasize that more research is necessary to determine whether those newly classified under the EASO definition would truly benefit from targeted obesity treatment.
Expert Perspective
In an accompanying editorial, Dr. Christina C. Wee, senior deputy editor of Annals of Internal Medicine, acknowledged the potential value of the EASO framework but stressed the need for further study. She noted that to build consensus on a universal definition of obesity, researchers must directly compare various classification methods in diverse populations.
Wee also highlighted that any globally applicable system must:
-
Use accessible, low-cost, and reproducible measurements
-
Be feasible in both high- and low-resource settings
-
Maintain standardized, consistent measurement practices
Funding and Disclosures
The study was supported by Ariel University and the Holon Institute of Technology.
-
Dror Dicker disclosed receiving grants, honoraria, and advisory roles with companies including AstraZeneca, Boehringer-Ingelheim, Eli Lilly, and Novo Nordisk, as well as holding positions in EFIM and EASO.
-
Dr. Wee served as faculty at the Internal Medicine Meeting 2025. Additional disclosures for other authors are detailed in the publication.